In this coffee chat, Oami Amarasingham, Deputy Director of the Massachusetts Public Health Association, shares tips and insights to help participants learn how to successfully engage decision-makers to advance prevention.
Topic: Healthy Eating
Coffee Chat: Nutrition Strategies that Cost-Effectively Improve Population Health & Health Equity
In this coffee chat, Dr. Steven Gortmaker, Director of the Prevention Research Center on Nutrition and Physical Activity at the Harvard T.H. Chan School of Public Health and Principal Investigator of the CHOICES Project, describes two promising paths to reduce health disparities and improve health equity.
Strategy Profile: Creating Healthier Afterschool Environments

The information in this resource is intended only to provide educational information. This profile describes the estimated benefits, activities, resources, and leadership needed to implement a strategy to improve child health. This information can be useful for planning and prioritization purposes.
- Creating healthier afterschool environments is a strategy to improve nutrition and physical activity policies & practices through the Out of School Nutrition and Physical Activity (OSNAP) initiative for children in grades K-5 attending state-administered 21st Century Learning afterschool programs.
What population benefits?
Children in grades K-5 attending state-administered 21st Century Learning afterschool programs.
What are the estimated benefits?
Relative to not implementing the strategy
Increase vigorous physical activity and improve nutritional quality of snacks and beverages offered in afterschool programs, and, in turn, promote healthy child weight.
What activities and resources are needed?
| Activities | Resources | Who Leads? |
| Issue regulations to improve nutrition and physical activity policies and practices in afterschool programs | • Time to issue and communicate regulations | State government |
| Provide training and technical assistance to regional Healthy Afterschool trainers on how to lead learning collaborative sessions | • Time for state Healthy Afterschool coordinator to lead trainings • Time for regional Healthy Afterschool trainers to be trained and receive technical assistance • Travel costs • Training material costs |
State healthy afterschool coordinator |
| Conduct regional learning collaboratives with afterschool program staff including training and technical assistance on goals and implementation activities | • Time for regional Healthy Afterschool trainers to lead learning collaboratives and provide technical assistance • Time for afterschool program staff to attend learning collaboratives and receive technical assistance • Training material costs • Travel costs |
Regional healthy afterschool trainer |
| Assess and implement actions to change program practices to meet Healthy Afterschool standards | • Time for afterschool program staff to conduct program practice self-assessments and implement changes at their program • Increase in food costs to provide snacks in compliance with nutrition standards to children attending Healthy Afterschool programs |
Afterschool program director |
| Develop CEU-accredited course for local program staff | • Cost to create a CEU-accredited course | State healthy afterschool coordinator |
| Provide educational materials and incentives to local program staff | • Material and incentive costs | State government |
| Monitor compliance to ensure afterschool programs are following programmatic requirements | • Time for state monitoring and compliance staff to monitor compliance • Travel costs |
State government monitoring and compliance staff |
| Establish a Healthy Afterschool recognition and monitoring website | • Time to create and maintain website | State government website developer |
Strategy Modification
This strategy could be modified to benefit children who participate in out-of-school programs administered by other organizations (e.g., YMCA or Boys and Girls Club of America). With this modification, the activities necessary to carry out the voluntary recognition program may not be included (e.g., issuing regulations, creating a healthy afterschool nutrition website, and monitoring compliance). With this modification, the impact on health is expected to be similar, and the impact on reach and cost may vary.
FOR ADDITIONAL INFORMATION
Cradock AL, Barrett JL, Kenney EL, Giles CM, Ward ZJ, Long MW, Resch SC, Pipito AA, Wei ER, Gortmaker SL. Using cost-effectiveness analysis to prioritize policy and programmatic approaches to physical activity promotion and obesity prevention in childhood. Prev Med. 2017 Feb;95 Suppl: S17-S27. doi: 10.1016/j.ypmed.2016.10.017. Supplemental Appendix with strategy details available at: https://ars.els-cdn.com/ content/image/1-s2.0-S0091743516303395-mmc1.docx
- Browse more CHOICES research briefs & reports in the CHOICES Resource Library.
- Explore and compare this strategy with other strategies on the CHOICES National Action Kit.
Suggested Citation
CHOICES Strategy Profile: Creating Healthier Afterschool Environments. CHOICES Project Team at the Harvard T.H. Chan School of Public Health, Boston, MA; May 2023.
Funding
This work is supported by The JPB Foundation and the Centers for Disease Control and Prevention (U48DP006376). The information provided here is intended to be used for educational purposes. Links to other resources and websites are intended to provide additional information aligned with this educational purpose. The findings and conclusions are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention or other funders.
Adapted from the TIDieR (Template for Intervention Description and Replication) Checklist
Coffee Chat: Tips & Resources for Communicating about Public Health Nutrition
In this coffee chat, Brett Otis, ALM, Nutrition Communications Project Manager in the Department of Nutrition at the Harvard T.H. Chan School of Public Health, shares tips and resources to communicate about public health. Those working in public health – particularly in the nutrition field – face many challenges when trying to communicate accurately and effectively about science- and evidence-based information.
View the resource round-up from this coffee chat.
February 2022 Coffee Chat Resource Round-Up
This document compiles resources and information shared during the February 24, 2022 coffee chat, which featured partners who shared creative ways they have brought attention to prevention and health promotion priorities in their communities.
May 2021 Coffee Chat Resource Round-Up
A collection of health equity promotion resources shared by CHOICES Community of Practice members during the May 2021 coffee chat.
Brief: Creating Healthier Child Care Environments: NAPSACC in the Quality Rating Improvement System in Arkansas

The information in this brief is intended only to provide educational information.
This brief summarizes a CHOICES Learning Collaborative Partnership model examining a strategy incorporating the Nutrition and Physical Activity Self-Assessment for Child Care (NAP SACC) assessment tools into Better Beginnings, Arkansas’ Quality Rating and Improvement System, to support quality early child care program opportunities and promote child health.
The Issue
In Arkansas, three out of 10 kindergarteners entering school in 2018 had overweight or obesity.1 The majority of today’s children will have obesity at age 35 if we don’t act.2 Making sure children are growing up at a healthy weight from their very first days is a critical way to prevent obesity and future risk for obesity-related diseases like diabetes as adults. Conditions linked to obesity, previously only seen in adults, are appearing in Arkansas’ Medicaid-enrolled children.3 Early child care programs that support healthy nutrition and physical activity habits show great promise in promoting healthy weight.4
In Arkansas, more than half of children ages 2-5 attend a licensed child care program.5 Providing licensed child care programs with training opportunities and resources through Better Beginnings may be an effective strategy to improve the quality of child care programs and to ensure that the majority of children in Arkansas are off to a healthy start.
About NAP SACC
NAP SACC is an evidence-based, trusted strategy enabling child care centers to attain best practices regarding nutrition, active play, and screen time.4 To date, NAP SACC shows the best evidence for reducing childhood obesity risk in children under age 5.6 Early education program directors and staff complete self-assessments and receive training and technical assistance to implement practices, policies, and changes supporting healthy outcomes. Better Beginnings is designed to improve child care environments to support child health and development. Integrating NAP SACC into Better Beginnings can improve the quality of child care programs and ensure more children grow up healthy in Arkansas.
Comparing Costs and Outcomes
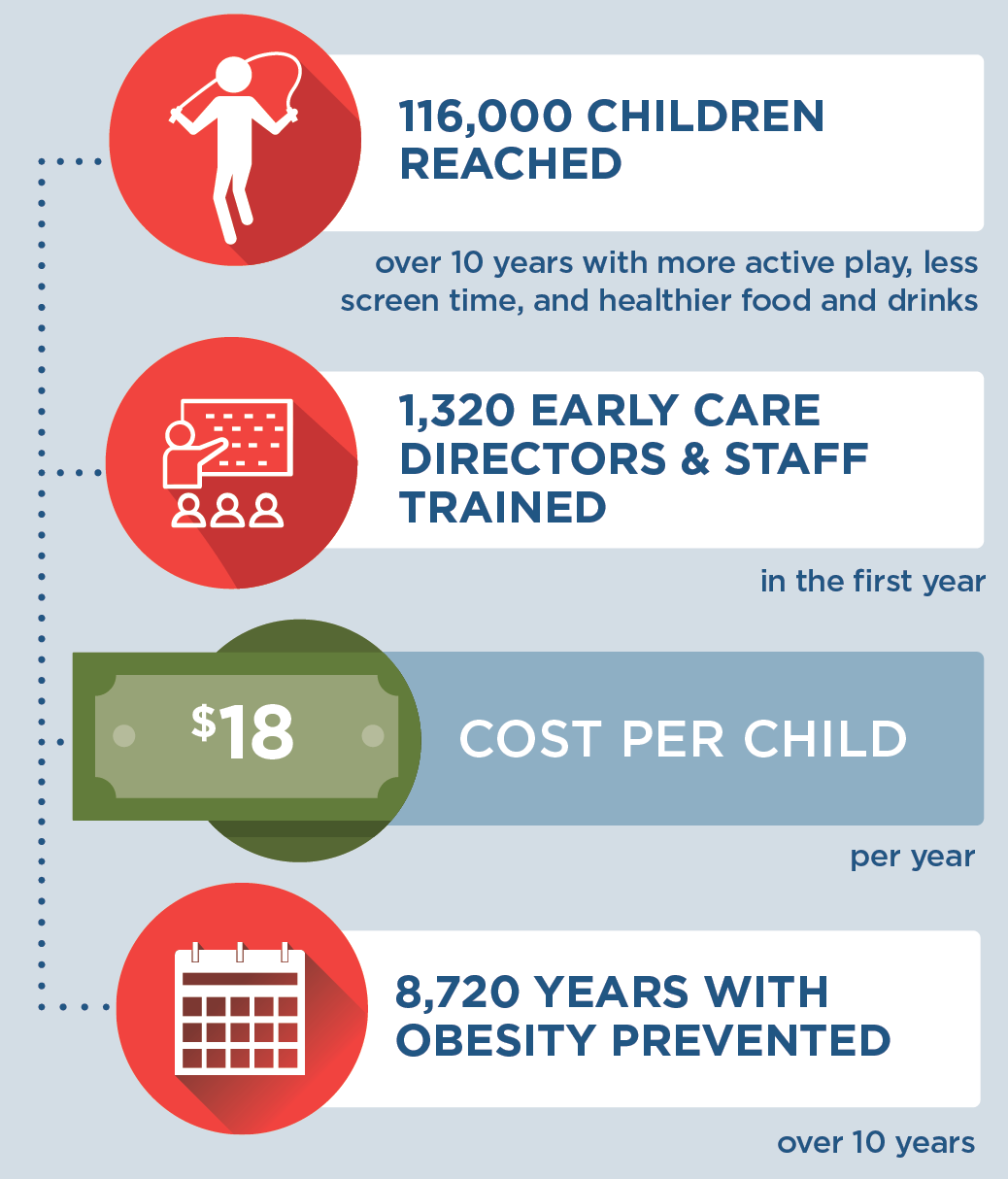
A CHOICES cost-effectiveness analysis compared the costs and outcomes over a 10-year time horizon (2020-2030) of implementing NAP SACC with the costs and outcomes of not implementing the program.
|
Implementing NAP SACC into Better Beginnings in Arkansas is an investment in child health. By the end of 2030: |
Conclusions and Implications
Every child should have opportunities for a healthy start. A state-level initiative integrating NAP SACC into training and quality improvement through Better Beginnings could create healthier nutrition and physical activity environments in child care programs for 116,000 children over 10 years. This strategy would benefit 1,320 early care directors and staff with training and technical assistance to support using nutrition, active play, and screen time best practices at 659 child care programs. Over 10 years, children in Arkansas would have 8,720 more years lived at a healthy weight and 1,130 fewer children would have obesity in 2030 alone.
Many prevention strategies targeting children require an upfront investment because costly obesity-related health conditions generally present later in adulthood.7 While we project this strategy would cost $18 per child per year, shortchanging early prevention efforts may lead to costly and complicated treatment in the future. Already, the total annual costs of having obesity are estimated to be $6 million for the 30,000 25- to 29-year-olds enrolled in Medicaid—inclusive of Arkansas’ expansion population. This represents an excess annual cost of $200 per person due to obesity.3
Early child care programs also play a critical role in supporting healthy child development and children’s academic readiness.8 Investing in a strategy for quality improvement that provides the necessary training, technical assistance, and resources supports early educators in providing high-quality child care that nurtures healthy habits. Enabling early education leaders in Arkansas to use the best available evidence to prevent excess weight gain in children will support children’s healthy growth and development.
References
-
ACHI. (2019). Assessment of Childhood and Adolescent Obesity in Arkansas: Year 16 (Fall 2018–Spring 2019). Arkansas Center for Health Improvement. Little Rock, AR.
-
Ward Z, Long M, Resch S, Giles C, Cradock A, Gortmaker S. Simulation of Growth Trajectories of Childhood Obesity into Adulthood. New England Journal of Medicine. 2017; 377(22): 2145-2153.
-
ACHI, Arkansas Medicaid. Comorbid Conditions and Medicaid Costs Associated with Childhood Obesity in Arkansas. 2019.
-
Alkon A, Crowley AA, Neelon SE, Hill S, Pan Y, Nguyen V, Rose R, Savage E, Forestieri N, Shipman L, Kotch JB. Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children’s body mass index. BMC Public Health. 2014;14:215.
-
Arkansas Department of Human Services, Division of Child Care and Early Childhood Education, Child Care Facilities Database. Unpublished data. 2020.
-
Kenney E, Cradock A, Resch S, Giles C, Gortmaker S. The Cost-Effectiveness of Interventions for Reducing Obesity among Young Children through Healthy Eating, Physical Activity, and Screen Time. Durham, NC: Healthy Eating Research; 2019. Available at: http://healthyeatingresearch.org
-
Gortmaker SL, Wang YC, Long MW, Giles CM, Ward ZJ, Barrett JL, …Cradock, AL. Three interventions that reduce childhood obesity are projected to save more than they cost to implement. Health Affairs. 2015; 34(11), 1932–1939.
-
Morrisey T. The Effects of Early Care And Education on Children’s Health. Health Affairs Health Policy Brief. 2019
Suggested Citation:Adams B, Sutphin B, Betancourt K, Balamurugan A, Kim H, Bolton A, Barrett J, Reiner J, Cradock AL. Arkansas: Creating Healthier Child Care Environments: Nutrition and Physical Activity Self-Assessment for Child Care (NAP SACC) in the Quality Rating Improvement System (QRIS) {Issue Brief}. Arkansas Department of Health, Little Rock, AR, and the CHOICES Learning Collaborative Partnership at the Harvard T.H. Chan School of Public Health, Boston, MA; May 2021. For more information, please visit www.choicesproject.org |
The design for this brief and its graphics were developed by Molly Garrone, MA and partners at Burness.
This issue brief was developed at the Harvard T.H. Chan School of Public Health in collaboration with the Arkansas Department of Health through participation in the Childhood Obesity Intervention Cost-Effectiveness Study (CHOICES) Learning Collaborative Partnership. This brief is intended for educational use only. This work is supported by The JPB Foundation and the Centers for Disease Control and Prevention (U48DP006376). The findings and conclusions are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention or other funders.
Making CHOICES in a Health Department: Case 2 (Advanced)

In this advanced teaching case, which builds on Case 1, a fictional health department continues to work with the CHOICES Project’s Learning Collaborative Partnership to determine how to implement an evidence-based strategy that requires substantial investment, but they face a variety of additional challenges such as state politics and the complexities of health policy.
Making CHOICES in a Health Department: Case 1 (Introductory)

In this introductory teaching case, a fictional health department engages with the CHOICES Project’s Learning Collaborative Partnership to help them narrow down a list of potential strategies to reduce childhood obesity in their county through a cost-effectiveness lens.
Impact Of The Healthy, Hunger-Free Kids Act On Obesity Trends

A CHOICES study examined the impact of the Healthy, Hunger-Free Kids Act of 2010 on child obesity risk, and found that policies that strengthen nutritional standards for meals and beverages at schools may be effective tools for reducing obesity among children living in poverty.
Kenney EL, Barrett JL, Bleich SN, Ward ZJ, Cradock AL, Gortmaker SL. Impact Of The Healthy, Hunger-Free Kids Act On Obesity Trends. Health Aff. 2020;39(7). doi:10.1377/hlthaff.2020.00133

The study’s research team, led by Erica Kenney, examined the impact of the Healthy, Hunger-Free Kids Act of 2010 on child obesity risk. The legislation strengthened nutritional standards for meals and beverages provided through the National School Lunch, Breakfast, and Smart Snacks programs. The Act’s whole grain standards were relaxed under the Trump administration, but this change was struck down in federal court. Additional rollbacks of the Act’s standards have been proposed.
The researchers reviewed data for 173,013 youths taken from the National Survey of Children’s Health from 2003–2018, prior to when rollbacks went into effect.
While they found no significant association between the legislation and childhood obesity trends overall, they did find significant reductions in obesity risk among children living in poverty—a population that is particularly reliant on school meals. Among these children, the risk of obesity, which had been trending steadily upwards prior to the legislation going into effect, declined substantially each year following the act’s implementation, translating to a 47% reduction in obesity prevalence in 2018 from what would have been expected without the legislation.
The researchers conclude that the Healthy, Hunger-Free Kids Act’s science-based nutritional standards should be maintained to support healthy growth, especially among children living in poverty. They also suggest that policymakers consider strategies to increase participation in school meals programs.
“Based on our study, as well as research that USDA and other researchers have conducted showing improvements in diet, the improved school meals standards have been a great public health success story,” said first author Kenney. “These healthier school meals are helping to protect the health of the children who have been placed at highest risk for poor health, and they reduce hunger while also reducing their risk of chronic diseases later in life.”