The information in this resource is intended only to provide educational information. This profile describes the estimated benefits, activities, resources, and leadership needed to implement a strategy to improve child health. This information can be useful for planning and prioritization purposes.
- Active Recess is a program to increase physical activity during elementary school recess with structured activities, playground markings, and/or portable play equipment. This program is implemented in elementary schools to promote physical activity during recess.
What population benefits?
Children in grades K-5 (5-11 years old).
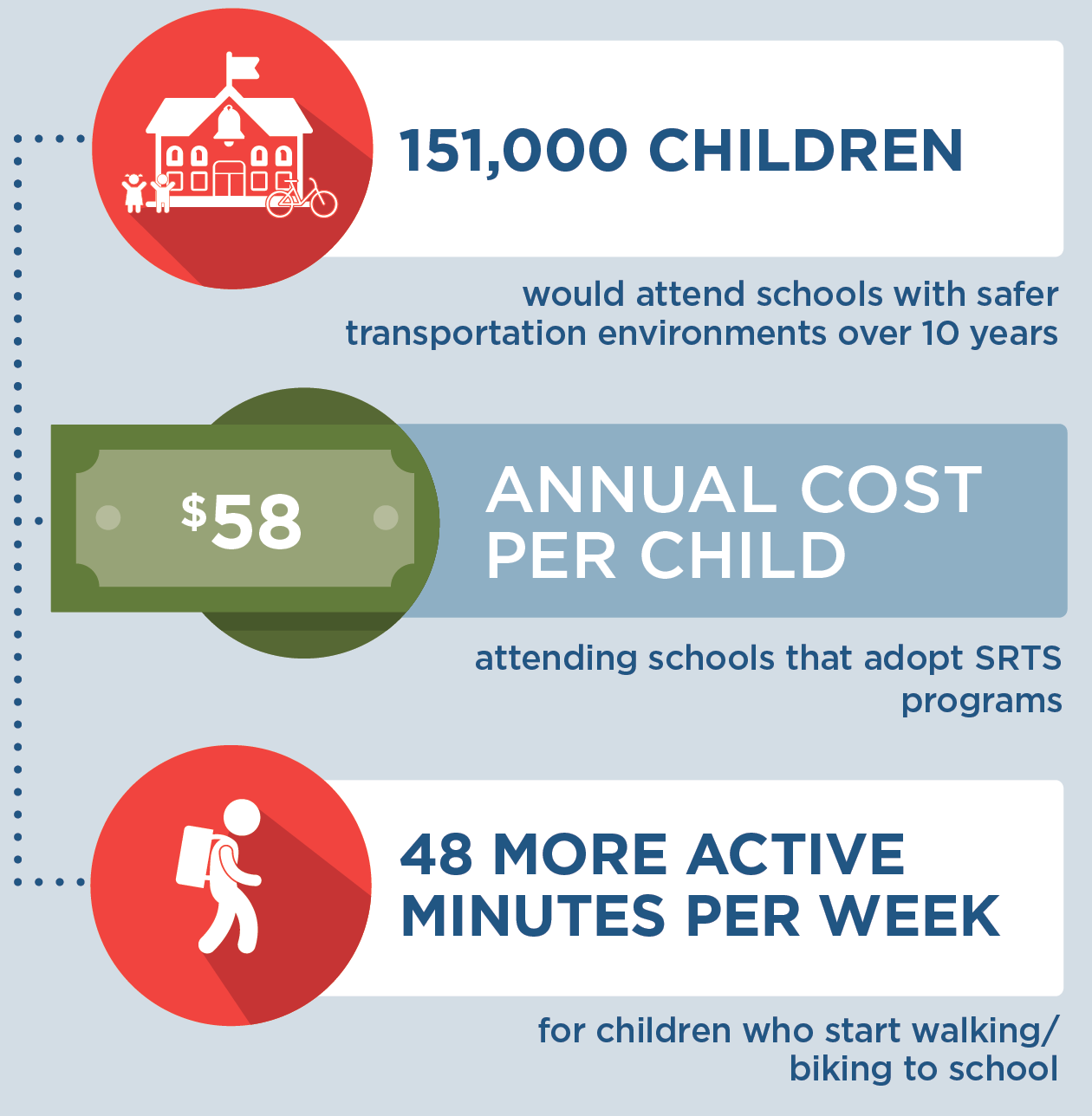
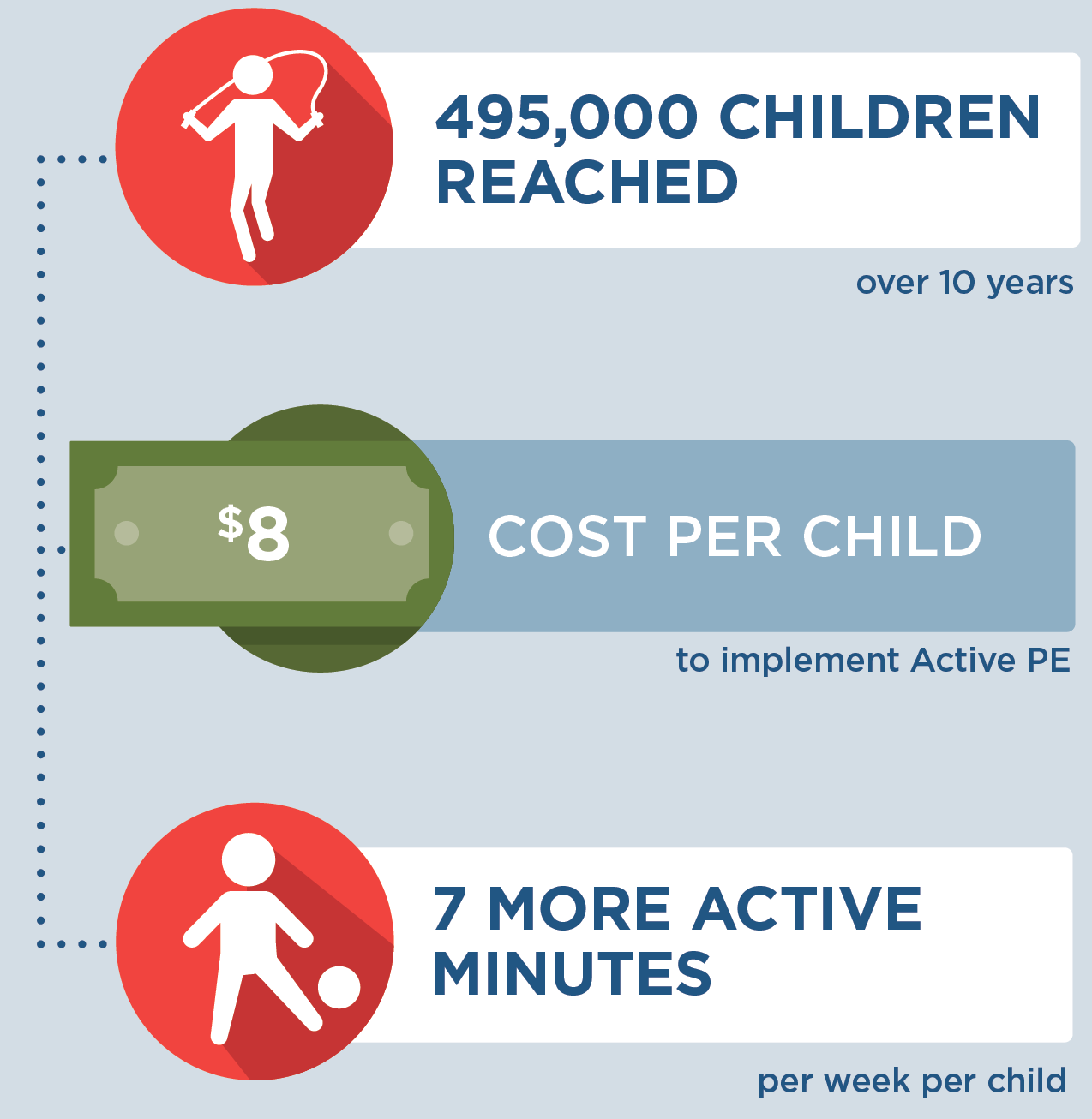
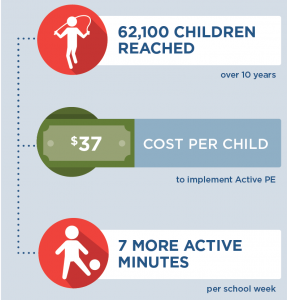
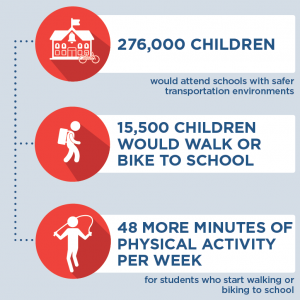
What are the estimated benefits?
Relative to not implementing the strategy
Increase students’ moderate-to-vigorous physical activity levels and, in turn, promote healthy child weight.
What activities and resources are needed?
| Activities | Resources | Who Leads? |
| Train teachers and recess monitors on recess supervision strategies to increase physical activity | • Time for trainer to lead trainings on supervision strategies to increase physical activity • Time for teachers and recess monitors to attend trainings • Travel costs for the trainers, teachers, and recess monitors |
School district coordinator |
| Paint markings onto outdoor play spaces | • Time for volunteers to paint markings • Time for school staff member to supervise painting • Painting material costs |
School staff member |
| Purchase portable playground equipment | • Playground equipment costs | Schools |
Strategy Modification
Some state and local health agencies have added to this strategy the costs of coordinating a broader state-level program when envisioning it being implemented in more than one district. This would add time for a state-level coordinator in the Department of Education to oversee the program and provide training to participating district-level coordinators. With this modification, this strategy could reach more children.
FOR ADDITIONAL INFORMATION
Cradock AL, Barrett JL, Kenney EL, Giles CM, Ward ZJ, Long MW, Resch SC, Pipito AA, Wei ER, Gortmaker SL. Using cost-effectiveness analysis to prioritize policy and programmatic approaches to physical activity promotion and obesity prevention in childhood. Prev Med. 2017 Feb;95 Suppl: S17-S27. doi: 10.1016/j.ypmed.2016.10.017. Supplemental Appendix with strategy details available at: https://ars.els-cdn.com/ content/image/1-s2.0-S0091743516303395-mmc1.docx
Selected CHOICES research brief including cost-effectiveness metrics:
McKinnon A, Barrett J, Cradock AL, Flax C. Salt Lake County: Active Recess {Issue Brief}. Salt Lake County Health Department, Salt Lake City, UT, and the CHOICES Learning Collaborative Partnership at the Harvard T.H. Chan School of Public Health, Boston, MA; December 2019. Available at: https://choicesproject.org/publications/brief-active-recess-salt-lake-county/
- Browse more CHOICES research briefs & reports in the CHOICES Resource Library.
- Explore and compare this strategy with other strategies on the CHOICES National Action Kit.
Suggested Citation
CHOICES Strategy Profile: Active Recess. CHOICES Project Team at the Harvard T.H. Chan School of Public Health, Boston, MA; April 2022.
Funding
This work is supported by The JPB Foundation and the Centers for Disease Control and Prevention (U48DP006376). The information provided here is intended to be used for educational purposes. Links to other resources and websites are intended to provide additional information aligned with this educational purpose. The findings and conclusions are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention or other funders.
Adapted from the TIDieR (Template for Intervention Description and Replication) Checklist