Dr. Stephen Resch describes why cost analyses can be useful, what key costing perspectives and principles are, and what the CHOICES methods and approach for defining and identifying strategy components, activities, and resources are.
Posted on July 10, 2020
Dr. Stephen Resch describes why cost analyses can be useful, what key costing perspectives and principles are, and what the CHOICES methods and approach for defining and identifying strategy components, activities, and resources are.
Posted on July 7, 2020

A CHOICES study examined the impact of the Healthy, Hunger-Free Kids Act of 2010 on child obesity risk, and found that policies that strengthen nutritional standards for meals and beverages at schools may be effective tools for reducing obesity among children living in poverty.
Kenney EL, Barrett JL, Bleich SN, Ward ZJ, Cradock AL, Gortmaker SL. Impact Of The Healthy, Hunger-Free Kids Act On Obesity Trends. Health Aff. 2020;39(7). doi:10.1377/hlthaff.2020.00133

The study’s research team, led by Erica Kenney, examined the impact of the Healthy, Hunger-Free Kids Act of 2010 on child obesity risk. The legislation strengthened nutritional standards for meals and beverages provided through the National School Lunch, Breakfast, and Smart Snacks programs. The Act’s whole grain standards were relaxed under the Trump administration, but this change was struck down in federal court. Additional rollbacks of the Act’s standards have been proposed.
The researchers reviewed data for 173,013 youths taken from the National Survey of Children’s Health from 2003–2018, prior to when rollbacks went into effect.
While they found no significant association between the legislation and childhood obesity trends overall, they did find significant reductions in obesity risk among children living in poverty—a population that is particularly reliant on school meals. Among these children, the risk of obesity, which had been trending steadily upwards prior to the legislation going into effect, declined substantially each year following the act’s implementation, translating to a 47% reduction in obesity prevalence in 2018 from what would have been expected without the legislation.
The researchers conclude that the Healthy, Hunger-Free Kids Act’s science-based nutritional standards should be maintained to support healthy growth, especially among children living in poverty. They also suggest that policymakers consider strategies to increase participation in school meals programs.
“Based on our study, as well as research that USDA and other researchers have conducted showing improvements in diet, the improved school meals standards have been a great public health success story,” said first author Kenney. “These healthier school meals are helping to protect the health of the children who have been placed at highest risk for poor health, and they reduce hunger while also reducing their risk of chronic diseases later in life.”
Posted on June 29, 2020
Dr. Steve Gortmaker provides an overview of the CHOICES Project, discussing both the methods and goals of the project.
Posted on June 26, 2020
Dr. Erica Kenney discusses the importance of quantitative estimates for behavior and BMI change, how the CHOICES team determines the quality of research evidence, and how the strategy-health pathway is used to estimate a strategy’s impact on health.
Posted on June 26, 2020
Dr. Angie Cradock describes the CHOICES methods for estimating strategy reach and identifying reach data sources.
Posted on May 18, 2020
Definitions for all CHOICES effect, cost, reach, and cost-effectiveness metrics.
Posted on May 18, 2020
Key differences between cost-effectiveness analysis and cost-benefit analysis.
Posted on May 18, 2020
Lead author of “Simulation of Growth Trajectories of Childhood Obesity into Adulthood” (NEJM 2017) Zach Ward talks about predicting the future of childhood obesity.
Forecasting Trends in Child Obesity with Zach Ward from CHDS Media Hub on Vimeo.
Posted on December 19, 2019
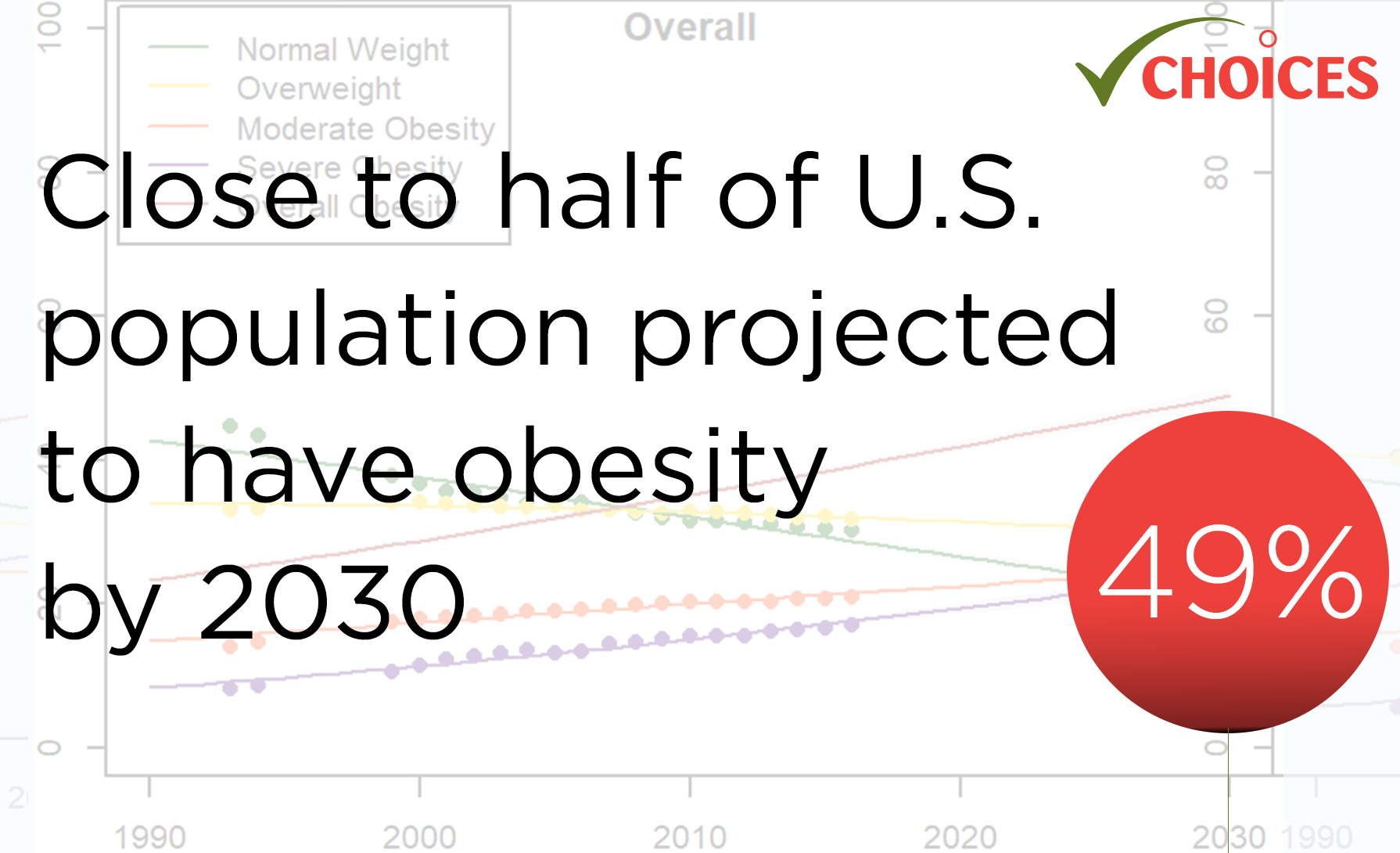
A CHOICES study finds that about half of the adult U.S. population will have obesity and about a quarter will have severe obesity by 2030. Severe obesity—once a rare condition—is projected to be the most common BMI category in 10 states and in some demographic subgroups.
Ward ZJ, Bleich SN, Cradock AL, Barrett JL, Giles CM, Flax CN, Long MW, Gortmaker SL. Projected U.S. State-Level Prevalence of Adult Obesity and Severe Obesity. N Engl J Med. 2019;381:2440-50. doi: 10.1056/NEJMsa1909301
According to this CHOICES study, about half of the adult U.S. population will have obesity and about a quarter will have severe obesity by 2030. The study also predicts that in 29 states, more than half of the population will have obesity, and all states will have a prevalence of obesity higher than 35%. The study’s researchers estimate that, currently, 40% of American adults have obesity and 18% have severe obesity.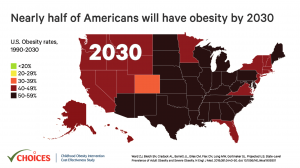
The researchers said the predictions are troubling because the health and economic effects of obesity and severe obesity take a toll on several aspects of society.
“Obesity, and especially severe obesity, are associated with increased rates of chronic disease and medical spending, and have negative consequences for life expectancy,” said Steven Gortmaker, Professor of the Practice of Health Sociology at the Harvard T.H. Chan School of Public Health and senior author of the study.
For the study, the researchers used self-reported body mass index (BMI) data from more than 6.2 million adults who participated in the Behavioral Risk Factor Surveillance System Survey (BRFSS) between 1993 and 2016. Body mass index (BMI) is calculated by dividing a person’s weight in kilograms by the square of their height in meters. Obesity is defined as a BMI of 30 or higher, and severe obesity is a BMI of 35 or higher. Self-reported BMIs are frequently biased, so the researchers used novel statistical methods to correct for this bias.
The large amount of data collected in the BRFSS allowed the researchers to drill down for obesity rates for specific states, income levels, and sub-populations. The results showed that by 2030, several states will have obesity prevalence close to 60%, while the lowest states will be approaching 40%. The researchers predicted that nationally, severe obesity will likely be the most common BMI category for women, non-Hispanic black adults, and those with annual incomes below $50,000 per year.
“The high projected prevalence of severe obesity among low-income adults has substantial implications for future Medicaid costs,” said lead author Zachary Ward, Programmer/Analyst at the Harvard T.H. Chan School of Public Health’s Center for Health Decision Science. “In addition, the effect of weight stigma could have far-reaching implications for socioeconomic disparities as severe obesity becomes the most common BMI category among low-income adults in nearly every state.”
Ward and his co-authors said that the study could help inform state policy makers. For example, previous research suggests that sugary drink taxes have been an effective and cost-effective strategy for curtailing the rise in obesity rates. “Prevention is going to be key to better managing this epidemic,” said Ward.
|
 |
Lead author Zach Ward discusses the paper with the Center for Health Decision Science.
Posted on December 1, 2017
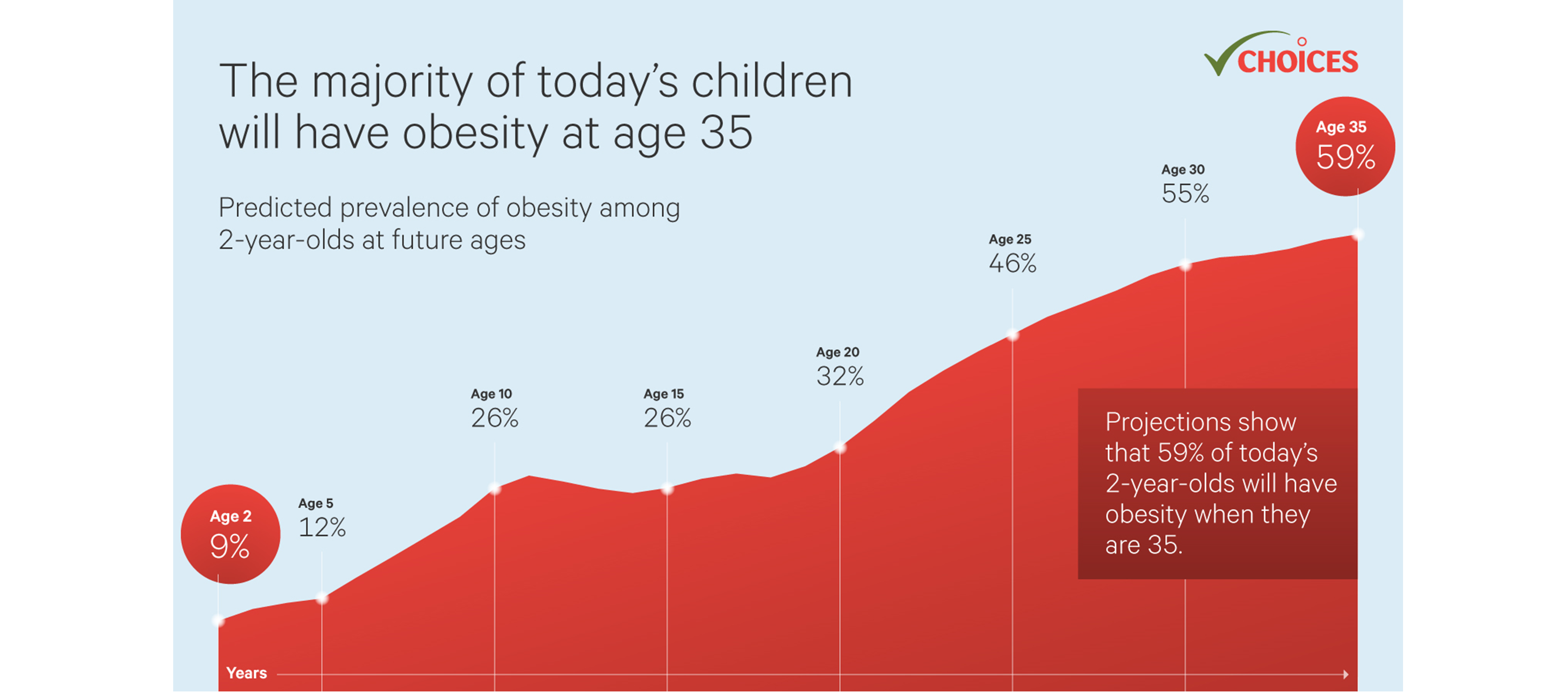
A CHOICES study finds that the obesity epidemic is far from over and is likely to become much worse, as study results predict that 57% of today’s children will have obesity at age 35. Public health professionals need to re-double their efforts to prevent such an outcome. The CHOICES Project has identified cost-effective interventions in school and community settings that can prevent future obesity cases.
Ward Z, Long M, Resch S, Giles C, Cradock A, Gortmaker S. Simulation of Growth Trajectories of Childhood Obesity into Adulthood. N Engl J Med. 2017 Nov 30;377(22):2145-2153.
The current childhood obesity epidemic has been well-documented, but more research is needed on the long-term risks for children. For this study, the researchers developed an individual-level simulation model for the current population of children in the U.S. that estimates the risk of adult obesity at age 35 years. Height and weight data were gathered from 5 nationally-representative longitudinal studies. The model, representative of the U.S. population in 2016, created 1,000 virtual populations of 1 million children each. Using this model with these virtual populations, obesity risk trajectories were projected up to the age of 35 years.
The researchers predict that, if nothing is done to change current trends, 57% of today’s children will have obesity at age 35. This is a large increase, given that 37% of adults now have obesity. In addition, the study found that excess weight in childhood is highly predictive of adult obesity. This is especially true for children with severe obesity, even at very young ages. The team estimated that 79% of two year-olds with severe obesity will still have obesity by the time they are 35 years old, as will 94% of 19 year-olds with severe obesity. Racial and ethnic disparities in obesity are already present by the age of two and persist into adulthood.
The results of this study reinforce some important public health messages.
“We find that obesity will be a significant problem for most children in the U.S. as they grow older,” said Zachary Ward, lead author on the study. “Given their increased risk of adult obesity, it seems clear that children who already have obesity are prime candidates for early intervention. However, even children currently at a healthy weight can benefit from preventive interventions, given the high risk of developing obesity in young adulthood.”
The team also noted that the findings of this study highlight the importance of promoting a healthy weight throughout childhood and into adulthood.
Given the high risk posed to children – especially those who already have obesity – public health professionals need to work to identify and implement effective strategies that focus on preventive interventions for all children. In previous work, the CHOICES team has identified a number of cost-effective interventions that with broad population reach. Such interventions focus on preventing excess weight gain starting at an early age by providing opportunities for healthier foods, beverages, and physical activity, such as within early care and education and school settings. Some of these interventions are projected to save more in future health care costs than they cost to implement.
See our news story for the full list of media coverage of this article.
Lead author Zach Ward discusses the paper with the Center for Health Decision Science.
Forecasting Trends in Child Obesity with Zach Ward from CHDS Media Hub on Vimeo.