
The information in this Story from the Field is intended only to provide educational information.
In this story from the field, partners at Denver Health worked with the CHOICES Team to see what might happen if they made changes to their electronic medical record systems to prompt pediatric medical providers to recognize children with too much weight for their health during well-child visits, and provide follow-up supportive care, education, and educational messages to families.
Identifying Priorities in Denver
Two departments of Denver Health – Denver Public Health and Community Health Services – identified healthy weight as a goal of their local Community Health Improvement Plan to address local population health priorities. Many partners had several ongoing initiatives to ensure that Denver’s children did not have too much weight for their health. As the health care provider for one-third of Denver’s children, Denver Health recognized its potential to reach more families by undertaking additional actions within its health system. Evidence suggests that racial, ethnic, and low-income groups in U.S. communities tend to have greater exposure to negative environmental influences and less access to protective factors, making maintaining a healthy weight more challenging.
Gathering Information for Action
In 2017, partners in Denver teamed up with the Childhood Obesity Intervention Cost-Effectiveness Study (CHOICES) Project at the Harvard T.H. Chan School of Public Health’s Learning Collaborative Partnership. The CHOICES Project works with health agencies to create new evidence to inform decision-making. Using local data, health agencies learn how to apply evaluations of effectiveness, reach, and cost to understand the relative cost-effectiveness of strategies to prevent and treat childhood obesity.
Strategy Selection
The Denver Learning Collaborative Partnership Team attended a CHOICES training and reviewed strategies to find best-value-for-money options for preventing children from having too much weight for health. One approach seemed particularly relevant: The Study of Technology to Accelerate Research (STAR), a clinical strategy that had been shown effective in a randomized trial.1
The Intervention
STAR uses decision support tools in the Epic electronic medical record system to help the health care team recognize and engage supports for children at annual well-child visits. Families receive education and can opt to receive text messages on healthy habits, like increasing physical activity and adopting healthier nutrition practices.
The Change Needed
While Denver Health had many pieces for STAR already in place, they would need several adjustments. Denver Health needed to modify its health record protocol to include diagnosis, screening, and decision support prompts for children with a BMI at or above 85%. Denver Health could build on its existing text messaging system and develop materials to provide relevant education and resources to parents and families, and then ensure training opportunities for pediatricians.
Steps Taken for Implementation
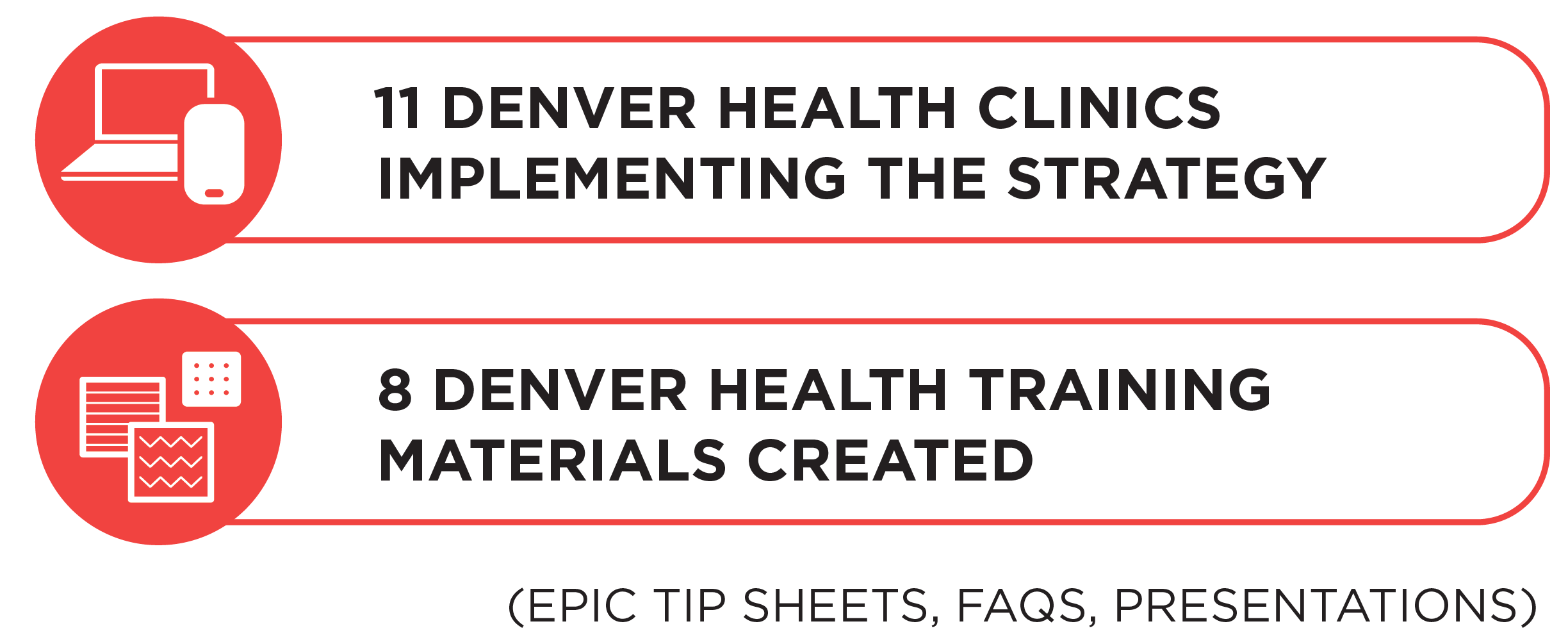
-
Interviewed clinicians to build engagement and incorporate feedback in Epic modifications to include decision support tools and prompts to help identify and manage children with too much weight for health
-
Surveyed families to inform educational content and text message program
-
Modified Epic to include decision support tools
-
Trained the health care team on the changes in Epic and the available resources for families
Helping Change Happen
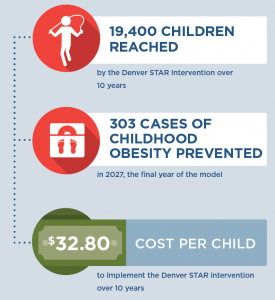
Through the CHOICES Learning Collaborative Partnership, the CHOICES Team works with local stakeholders to make projections about what may happen if they implement a program or policy. Here they calculated that STAR could reach 19,400 children in Denver over ten years and prevent 300 children from having too much weight for their health. For every dollar spent implementing STAR, $0.78 would be saved in health care costs because more children would have a healthier weight.2 This strategy is projected to both improve overall population health, as well as reduce disparities in too much weight for health among children. What’s more, this information gave Denver Health data to support a grant application for strategy implementation. With leadership support and funding, Denver Health was well positioned to begin implementing components from STAR in 2019.
Impact & Lessons Learned
With the STAR clinical strategy, it was so feasible compared to other strategies, and when looking at our entire budget, it is a drop in the overall bucket of funding.” – Jennifer Moreland, Chronic Disease Manager, Denver Public Health
References
-
Taveras E., Marshall R., Kleinman KP, Gillman MW, Hacker K…Simon SR. (2015). Comparative Effectiveness of Childhood Obesity Interventions in Pediatric Primary Care: A Cluster-Randomized Clinical Trial, JAMA Pediatrics, 169(6):535-542
-
Moreland J, Rosen J, Kraus E, Reiner J, Gortmaker S, Giles C, Ward Z. Denver: Study of Technology to Advance Research (STAR) [Issue Brief]. Denver Public Health and Denver Health, Denver, CO, and the CHOICES Learning Collaborative Partnership at the Harvard T.H. Chan School of Public Health, Boston, MA; July 2018.
Suggested Citation:CHOICES Stories from the Field: Denver Takes Action to Promote Healthy Child Weight. Denver Public Health, a Department of Denver Health, Denver, CO, and the CHOICES Project Team at the Harvard T.H. Chan School of Public Health, Boston, MA; October 2020. |



 “It is clear that the most cost-effective strategies for preventing new cases of obesity are population-level approaches like taxes and school-based policies,” said
“It is clear that the most cost-effective strategies for preventing new cases of obesity are population-level approaches like taxes and school-based policies,” said 