A CHOICES paper identifying cost-effective nutrition interventions with broad population reach highlights the importance of primary prevention for policy makers aiming to reduce childhood obesity.
Gortmaker SL, Claire Wang Y, Long MW, Giles CM, Ward ZJ, Barrett JL, Kenney EL, Sonneville KR, Afzal AS, Resch SC, Cradock AL. Three Interventions That Reduce Childhood Obesity Are Projected to Save More Than They Cost to Implement. Health Aff, 34, no. 11 (2015):1304-1311.
Reused with permission from Project HOPE/Health Affairs. The published article is archived and available online at www.healthaffairs.org.
The United States will not be able to treat its way out of the obesity epidemic with current clinical practice. Instead, reversing the tide of obesity will require expanded investment in primary prevention, focusing on a combination of interventions with broad population reach, proven individual effectiveness, and low cost of implementation.
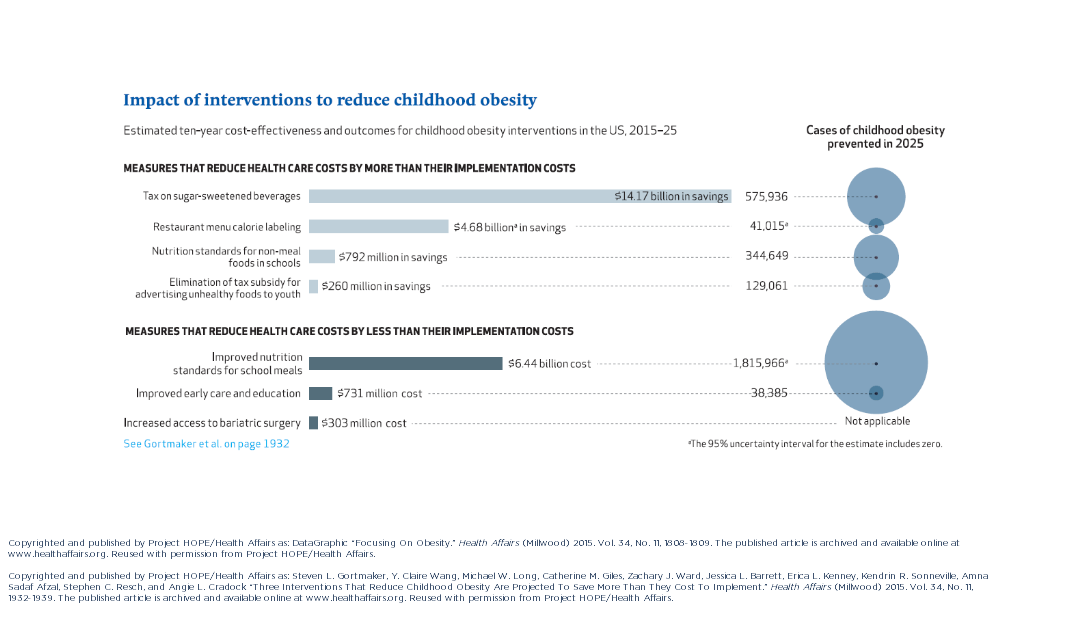
This study is the first of its kind to estimate the cost effectiveness of a wide variety of nutrition interventions high on the obesity policy agenda—documenting their potential reach, comparative effectiveness, implementation cost, and cost-effectiveness. Researchers identified three interventions that would more than pay for themselves by reducing healthcare costs related to obesity: an excise tax on sugar-sweetened beverages; elimination of the tax subsidy for advertising unhealthy food to children; and nutrition standards for food and drinks sold in schools outside of school meals. Implemented nationally, these interventions would prevent 576,000, 129,100, and 345,000 cases of childhood obesity, respectively, in 2025. The projected net savings to society in obesity-related health care costs for each dollar spent would be $30.78, $32.53, and $4.56, respectively.
Additional interventions modeled include restaurant menu calorie labeling, increased access to adolescent bariatric surgery, improved early care and education, and nutrition standards for school meals. The study points out that the improvements in nutrition standards for both school meals and foods and beverages sold outside of meals through current Smart Snacks in School regulation make the Healthy, Hunger-Free Kids Act of 2010 one of the most important national obesity prevention policy achievements in recent decades.
Though researchers analyzed interventions separately, no strategy on its own would be sufficient to reverse the obesity epidemic. The study also emphasizes the importance of obesity prevention that spans across multiple settings throughout the life course. While childhood interventions are necessary to reduce obesity during the early years of life and ensure that children enter into adulthood at a healthy weight, it is critical that environments spanning the life course continue to support healthy eating and drinking behaviors.
“Policy makers looking to reverse the childhood obesity epidemic and reduce long-term obesity prevalence need to focus on implementing cost-effective preventive interventions that reach a large percentage of our nation’s children,” says lead investigator of the CHOICES Project, Dr. Steve Gortmaker, who also serves as a Professor of the Practice of Health Sociology and the Director of the Prevention Research Center on Nutrition and Physical Activity at the Harvard T.H. Chan School of Public Health.
The study notes that interventions affecting both children and adults are particularly attractive, since near-term health care cost savings can be achieved by reducing adult obesity, while laying the ground work for long-term cost savings by reducing childhood obesity. The sugar-sweetened beverage excise tax, for example, would save $14.2 billion in net costs over the course of the decade, primarily due to reductions in adult health care costs.
Interventions that can achieve near-term health cost savings among adults and reduce childhood obesity offer policy makers an opportunity to make long-term investments in children’s health while generating short-term returns.

