The information in this brief is intended only to provide educational information.
This brief summarizes the findings from a CHOICES Learning Collaborative Partnership model examining a strategy to incorporate television time counseling into the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in Arkansas. WIC staff would be trained to assess children’s television viewing and offer education on modifying television behaviors during WIC certification visits.
The Issue
In Arkansas, three out of 10 kindergarteners entering school in 2018 had overweight or obesity.1 However, limiting children’s television viewing may help them grow up at a healthy weight because product marketing on television can lead children to consume too many unhealthy foods and drinks.2
The American Academy of Pediatrics recommends children view a maximum of one hour per day of quality screen programming.3 Yet, in 2019, many children ages 2-4 participating in Arkansas’ WIC program viewed twice that amount, averaging nearly two hours per day. Just two out of every 10 children viewed the recommended level of daily screen time.4
In Arkansas, the WIC program offers nutrition education, referrals, and supplemental food support to low-income families (in households with income less than 185% of poverty levels). Identifying strategies to help these families achieve the recommended levels of television would support children’s growth and development. Ensuring children are growing up at a healthy weight also increases their likelihood of having a healthy weight in adulthood.
About Women, Infants, and Children (WIC) Television Time Reduction
This evidence-based strategy involves training WIC clinic staff to assess television viewing practices and provide opportunities for counseling to caregivers to reduce the amount of television their child watches.5 This strategy would require a modification within the existing assessment tool used to personalize nutrition education, referrals, and food package tailoring that would prompt staff to ask caregivers questions during recertification visits and provide relevant educational resources and guidance. WIC clinic staff would be trained to ask caregivers how much television their children view and then share ways to reduce it.
Comparing Costs and Outcomes
CHOICES cost-effectiveness analysis compared the costs and outcomes over a 10-year time horizon (2020-2030) of implementing WIC Television Time Reduction with the costs and outcomes associated with not implementing the strategy.
|
Implementing WIC Television Time Reduction in Arkansas is an investment in the future. By the end of 2030: |
Conclusions and Implications
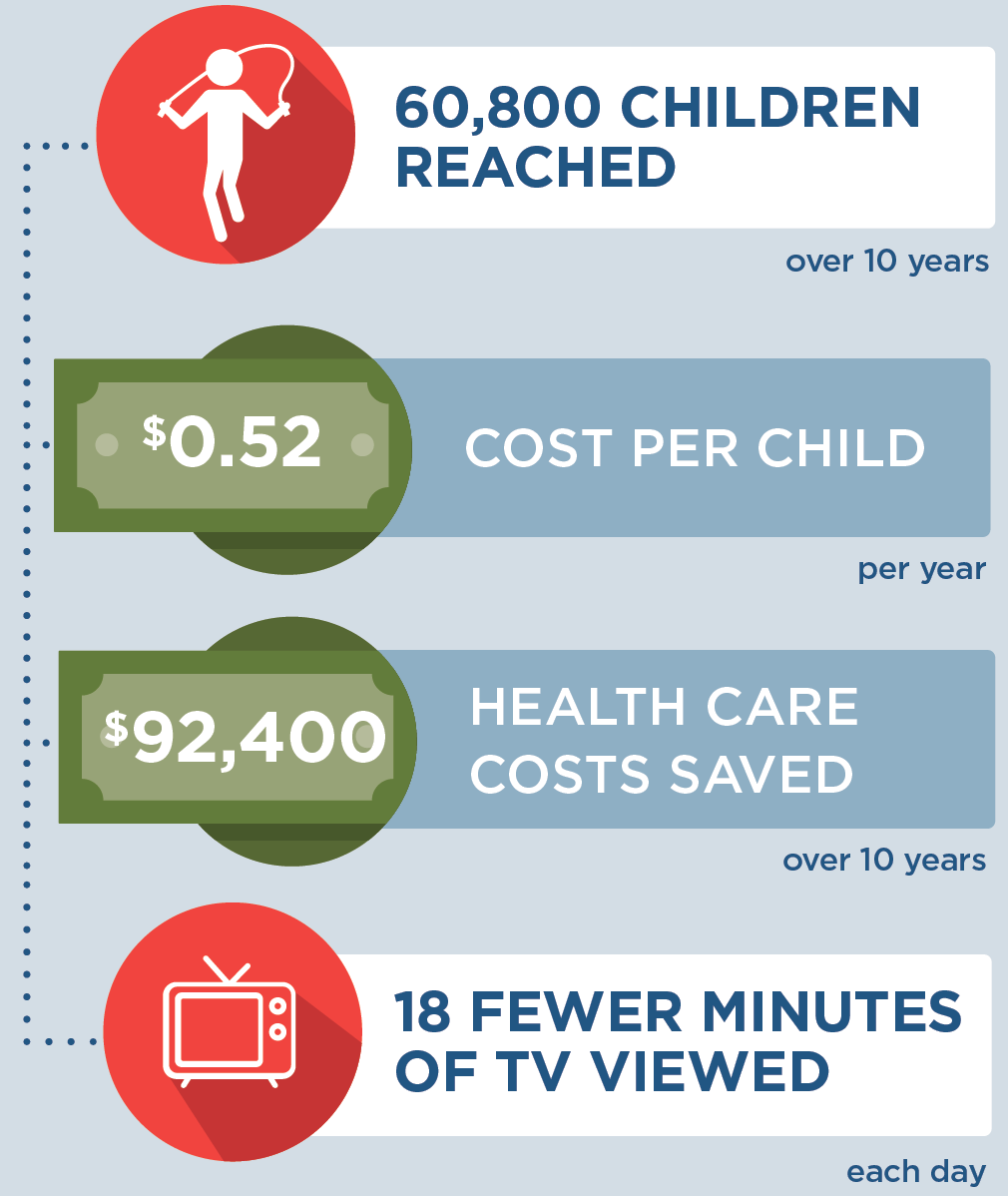
A state-level initiative that incorporates television viewing screening assessments and counseling practices into regular WIC visits could reach over 60,800 children and their families in Arkansas over 10 years. We project children would average 18 fewer minutes of television daily if these practices were incorporated. This strategy would prevent 314 cases of childhood obesity in Arkansas in 2030, at an average cost of $0.52 per child per year. Moreover, this investment in child health is estimated to pay off over 10 years. For every $1 spent on implementing this strategy, $1.06 in obesity-related health care costs would be saved over 10 years, saving $92,400 by 2030.
Children participating in WIC in Arkansas are in low-income households and are more likely to be Hispanic or Black than the general population of 2-4 year olds in Arkansas.4 CHOICES projected substantial reductions in cases of obesity among low-income children participating in WIC. Since this strategy is focused on populations with high risk of excess television viewing, and is not expected to impact obesity among higher income households not participating in WIC, it could lead to improvements in disparities in both television viewing and obesity risk.
The WIC program helps safeguard the health of children by providing supplemental foods, referrals, and nutrition education. These preventive strategies can play a critical role in helping children establish healthy habits early. Incorporating opportunities for skill-building to reduce television time into the WIC program is a low-cost and feasible strategy to ensure opportunities for more Arkansas children to grow up a healthy weight.
References
-
ACHI. Assessment of Childhood and Adolescent Obesity in Arkansas: Year 16 (Fall 2018-Spring 2019). Little Rock, AR: Arkansas Center for Health Improvement; 2019.
-
Russell SJ, Croker H, Viner RM. The effect of screen advertising on children’s dietary intake: A systematic review and meta-analysis. Obesity Reviews. 2019;20(4):554-568.
-
Council on Communications and Media. Media and Young Minds. Pediatrics. 2016;138(5):e20162591.
-
Arkansas Department of Health. WIC program 2019 data, unpublished report; accessed June 2020.
-
Whaley S, McGregor S, Jiang L, Gomez J, Harrison G, Jenks E. A WIC-Based Intervention to Prevent Early Childhood Overweight. Journal of Nutrition Education and Behavior. 2010 Feb; 52(3S) S47-51
Suggested Citation:Adams B, Sutphin B, Looney R, Rollins N, Balamurugan A, Kim H, Bolton A, Reiner J, Barrett J, Gortmaker SL, Cradock AL. Arkansas: Women, Infants, and Children (WIC) Television Time Reduction {Issue Brief}. Arkansas Department of Health, Little Rock, AR, and the CHOICES Learning Collaborative Partnership at the Harvard T.H. Chan School of Public Health, Boston, MA; May 2021. For more information, please visit www.choicesproject.org |
The design for this brief and its graphics were developed by Molly Garrone, MA and partners at Burness.
This issue brief was developed at the Harvard T.H. Chan School of Public Health in collaboration with the Arkansas Department of Health through participation in the Childhood Obesity Intervention Cost-Effectiveness Study (CHOICES) Learning Collaborative Partnership. This brief is intended for educational use only. This work is supported by The JPB Foundation and the Centers for Disease Control and Prevention (U48DP006376). The findings and conclusions are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention or other funders.