The information in this brief is intended for educational use only.
This brief summarizes a CHOICES Learning Collaborative Partnership simulation model in New Hampshire examining a potential strategy to expand child care providers’ access to the Nutrition and Physical Activity Self-Assessment for Child Care (Go NAP SACC) by targeting the state’s largest providers via contracted training and technical assistance.
The Issue
Over the past three decades, more and more people have developed obesity.1 Today, nearly nine percent of 2-5 year olds have obesity.2 Now labeled as an epidemic, health care costs for treating obesity-related conditions such as heart disease and diabetes were $147 billion in 2008.3 While multiple strategies are needed to reverse the epidemic, emerging prevention strategies directed at children show great promise.4 A large body of evidence shows that healthy eating, physical activity, and less time watching TV helps kids grow up at a healthy weight.
In New Hampshire, 40% of 2-5 year olds attend licensed child care centers; 24% attend a large center or family child care program.5 Making NAP SACC more available can encourage and empower programs to voluntarily improve nutrition, physical activity, and screen time standards.
About NAP SACC and Expanding Access for NH Child Care Programs
Go NAP SACC is an evidence-based, trusted intervention that helps child care programs improve practices for nutrition, active play, and screen time and can reduce childhood obesity.6,7 Child care providers complete self-assessments of their nutrition, active play, and screen time practices and receive training and technical assistance to implement self-selected changes to create healthier environments. Increasing the number of provider slots offered through a contract with child care training and technical assistance specialists at Keene State College, managed by New Hampshire’s Department of Health and Human Services, Division of Public Health Services (DPHS), could broaden the current reach of the Go NAP SACC project, allowing more licensed child care programs to improve nutrition and physical activity policies and practices. Currently, Keene State works with 22 child care providers. Since 2010, over ninety licensed child care programs, caring for nearly 8,000 children, have participated in DPHS funded opportunities to improve 465 nutrition and physical activity policies and practices.
Comparing Costs and Outcomes
CHOICES cost-effectiveness analysis compared the costs and outcomes of expanding New Hampshire’s NAP SACC program led by partners at Keene State College over 10 years.
Implementing NAP SACC in New Hampshire’s largest child care programs is an investment in the future. By the end of 2025: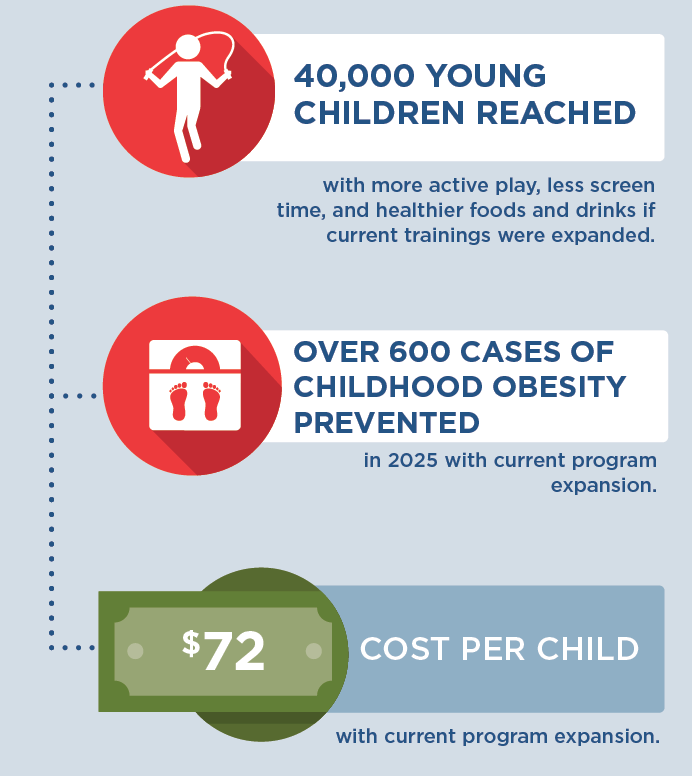 |
Conclusions and Implications
Every child deserves a healthy start in life. This includes ensuring that all kids in child care have opportunities to eat healthy foods and be physically active, no matter where they live or where they go for child care. A state-level initiative to bring NAP SACC to New Hampshire’s largest child care programs by expanding its current opportunities could prevent over 600 cases of childhood obesity in 2025 and ensure healthy child care environments for 40,000 young children.
A separate model examined the potential for expanding access to Go NAP SACC via the state’s Quality Rating Improvement System, which is a single-tiered system referred to as Licensed Plus. While such an initiative could be a useful policy tool for creating sustainable access to Go NAP SACC for NH child care providers, the results of that model indicated that fewer children (12,000) would be reached and fewer cases of obesity prevented in 2025 (100) at a slightly higher cost per child ($81). The results of the two models suggest that New Hampshire’s current contracted strategy targeting the state’s largest providers may be more cost-effective. Results from both models reinforce the importance of investing in prevention efforts to reduce the prevalence of obesity. Shortchanging prevention efforts can lead to more costly and complicated treatment options in the future, whereas introducing small changes to young children can help them develop healthy habits for life.
The first few years of childhood may be the best time to promote healthy eating behaviors in children. Programs such as Go NAP SACC lay the foundation by helping child care providers create environments to nurture healthy eating habits and increase opportunities for physical activity for all of the children.
References
- Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA. 2016 Jun 7;315(21):2284-91.
- Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, Flegal KM. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016 Jun 7;315(21):2292-9.
- Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual Medical Spending Attributable To Obesity: Payer-And Service-Specific Estimates. Health Affairs. 2009;28(5).
- Gortmaker SL, Wang YC, Long MW, Giles CM, Ward ZJ, Barrett JL, Kenney EL, Sonneville KR, Afzal AS, Resch SC, Cradock AL. Three interventions that reduce childhood obesity are projected to save more than they cost to implement. Health Aff (Millwood). 2015 Nov;34(11):1932-9.5
- Child Care Aware. State Child Care Facts in the State of New Hampshire, 2016. Accessed 8/17/17 at: http://childcareaware.org/wp-content/uploads/2016/08/New-Hampshire.pdf; Personal communication from NH Division of Public Health Services.
- Ward DS, Benjamin SE, Ammerman AS, Ball SC, Neelon BH, Bangdiwala SI. Nutrition and physical activity in child care: results from an environmental intervention. Am J Prev Med. 2008 Oct;35(4):352-6.
- Alkon A, Crowley AA, Neelon SE, Hill S, Pan Y, Nguyen V, Rose R, Savage E, Forestieri N, Shipman L, Kotch JB. Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children’s body mass index. BMC Public Health. 2014 Mar 1;14:215.
- Birch, L., Savage, J. S., & Ventura, A. (2007). Influences on the Development of Children’s Eating Behaviours: From Infancy to Adolescence. Canadian Journal of Dietetic Practice and Research : A Publication of Dietitians of Canada = Revue Canadienne de La Pratique et de La Recherche En Dietetique : Une Publication Des Dietetistes Du Canada, 68(1), s1–s56.
Suggested Citation:Kenney EL, Giles CM, Flax CN, Gortmaker SL, Cradock AL, Ward ZJ, Foster S, Hammond W. New Hampshire: Nutrition and Physical Activity Self-Assessment for Child Care (NAP SACC) Intervention {Issue Brief}. New Hampshire Department of Health and Human Services, Concord, NH, and the CHOICES Learning Collaborative Partnership at the Harvard T.H. Chan School of Public Health, Boston, MA; October 2017. |
The design for this brief and its graphics were developed by Molly Garrone, MA and partners at Burness.
This issue brief was developed at the Harvard T.H. Chan School of Public Health in collaboration with the New Hampshire Department of Health and Human Services through participation in the Childhood Obesity Intervention Cost-Effectiveness Study (CHOICES) Learning Collaborative Partnership. This brief is intended for educational use only. Funded by The JPB Foundation. Results are those of the authors and not the funders. For more information, please visit: https://www.dhhs.nh.gov
