The information in this brief is intended for educational use only.
This brief provides a summary of the CHOICES Learning Collaborative Partnership simulation model of a hypothetical requirement in Oklahoma’s Quality Rating and Improvement System, Reaching for the Stars, that family child care providers at or above Level 1.5 limit non-educational screen time for 2-5 year olds to 30 minutes daily.
The Issue
Over the past three decades, more and more people have developed obesity.1 Today, nearly nine percent of 2-5 year olds have obesity.2 Now labeled as an epidemic, health care costs for treating obesity-related health conditions such as heart disease and diabetes were $147 billion in 2008.3 While multiple strategies are needed to reverse the epidemic, emerging prevention strategies directed at children show great promise for addressing the epidemic.4 A large body of evidence shows that limiting time watching non-educational television helps kids grow up at a healthy weight. Research shows children watch nearly two hours of television daily at family child care programs.5
In Oklahoma, approximately 5.5% of 2-5 year olds attend a family child care program, and about 40% of those attend a program at Level 1.5 or higher in Reaching for the Stars.6 Quality improvement systems like Reaching for the Stars can support programs in creating a healthier screen time environment.
About the Policy to Help Licensing Care Programs to Reduce Screen Time
The policy to limit screen time in family child care settings to 30 minutes per day is based on national recommendations from pediatricians and child care and public health experts to limit screen time.7 Instituting the policy change through Reaching for the Stars would incentivize family child care programs to meet this standard, rather than mandating it. The policy change would also help support children’s development of healthy screen use habits.
Comparing Costs and Outcomes
CHOICES cost-effectiveness analysis compared the costs and outcomes of modifying the Reaching for the Stars standards to require the 30 min/day limit for family child care programs at level 1.5 or higher with costs and outcomes associated with not modifying the standards over 10 years.
Implementing screen time reduction policies in Oklahoma family child care programs is an investment in the future. By the end of 2025: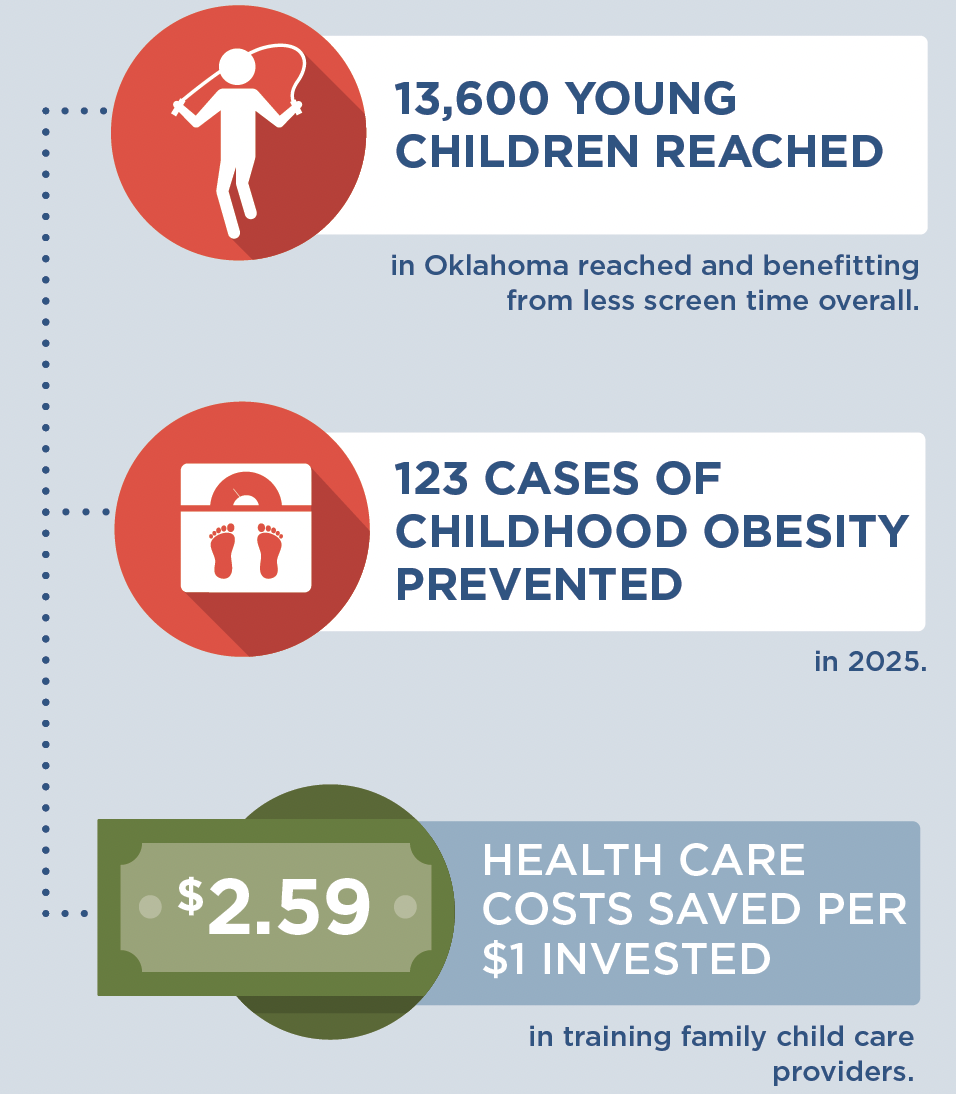 |
Conclusions and Implications
Every child deserves a healthy start in life. This includes ensuring that all children in child care have opportunities to be healthy, no matter where they live or where they go for child care. A state-level initiative to incentivize family child care providers to limit non-educational screen time in family child care settings could prevent 123 cases of childhood obesity in 2025 and ensure healthier child care environments for over 13,000 children.
What’s more, this inexpensive strategy would save Oklahoma money. For every $1.00 spent on implementing this screen time strategy, we would save $2.59 in health care costs. These results reinforce the importance of investing in prevention efforts, relative to other treatment interventions, to reduce the prevalence of obesity. Shortchanging prevention efforts can lead to more costly and complicated treatment options in the future, whereas introducing small changes to young children can help them develop healthy habits for life.
Evidence is growing about how to help children achieve a healthy weight. Programs to reduce screen time in child care are laying the foundation for a healthier future by helping child care providers create environments that nurture healthy habits. Leaders at the federal, state, and local levels should use the best available evidence to determine which evidence-based programs and policies hold the most promise to help children grow up at a healthy weight.
References
- Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA. 2016 Jun 7;315(21):2284-91.
- Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, Flegal KM. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016 Jun 7;315(21):2292-9.
- Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual Medical Spending Attributable To Obesity: Payer-And Service-Specific Estimates. Health Affairs. 2009;28(5).
- Gortmaker SL, Wang YC, Long MW, Giles CM, Ward ZJ, Barrett JL, Kenney EL, Sonneville KR, Afzal AS, Resch SC, Cradock AL. Three interventions that reduce childhood obesity are projected to save more than they cost to implement. Health Affairs (Millwood). 2015 Nov;34(11):1932-9.
- Tandon, P. S., Zhou, C., Lozano, P., & Christakis, D. A. (2011). Preschoolers’ total daily screen time at home and by type of child care. The Journal of Pediatrics, 158(2), 297-300
- Oklahoma Department of Health Services (DHS). Early Care & Education Licensing Database (2016)
- American Academy Of Pediatrics, American Public Health Association, National Resource Center for Health and Safety in Child Care and Early Education. Caring for our children: National health and safety performance standards; Guidelines for early care and education programs. 3rd edition. Elk Grove Village, IL: American Academy of Pediatrics; 2011
Suggested Citation:Case S, Simpson K, Khan F, U’ren S, Giles C, Kenney EL, Flax CN, Gortmaker SL, Ward ZJ, Cradock AL. Oklahoma: Updated Requirements in Reaching for the Stars to Reduce Non-Educational Screen Time for Young Children in Family Child Care Homes {Issue Brief}. Oklahoma State Department of Health and Oklahoma State Department of Human Services, Oklahoma City, OK, and the CHOICES Learning Collaborative Partnership at the Harvard T.H. Chan School of Public Health, Boston, MA; October 2017. |
|
The design for this brief and its graphics were developed by Molly Garrone, MA and partners at Burness. This issue brief was developed by the Oklahoma State Department of Health through participation in the Childhood Obesity Intervention Cost-Effectiveness Study (CHOICES) Learning Collaborative Partnership at the Harvard T.H. Chan School of Public Health. This brief is intended for educational use only. Funded by The JPB Foundation. Results are those of the authors and not the funders. |
